|
|||||||||||||||||||||||||||||
|

Dear Members and Friends of VSI, All vitiligo patients deserve respect, understanding, and access to effective treatments. However, many do not have that opportunity. From the inability to locate a doctor offering current vitiligo treatments, to the insurance companies who refuse to cover them, this is where a national organization like VSI is needed to proactively advocate on behalf of the entire vitiligo community. VSI's work on the national level is aimed at educating legislators and industry on the challenges that vitiligo patients regularly face and the need to establish policies, programs, and processes that eliminate the current barriers to treatment. We want you to know that your voice is being heard. A federal proposal to reduce Medicare's physician reimbursement rates is bringing doctors and patients from around the country together to help keep phototherapy available. VSI members and its leadership recently told federal policy makers about the importance for continued access to phototherapy. You can read more about this advocacy effort further on in this newsletter. Private insurers need to cover vitiligo treatments, and not impose excessive and unaffordable co-pays. VSI is collaborating with leading physicians to educate insurers around the country. To launch that campaign, we are asking our US members to complete the insurance survey included in this newsletter. The results will help us to develop and implement an informed and targeted strategy. Please participate in this survey – you will be making a difference. The voice and support of all who are affected by vitiligo are at the core of our ability to succeed. As a nonprofit organization, VSI depends on the financial support of the vitiligo community it serves to maintain our national presence. We are especially grateful to VSI members who recently sponsored and participated in fundraisers, a Sail-a-thon and a Walk-a-thon, to benefit VSI's programs and outreach. The Sail-a-thon was inspired by a father wanting to help change the future for his child. Vitiligo in children and teens can present special treatment issues, as well as unique self-esteem and identity challenges. Our main article in this newsletter focuses on childhood vitiligo. We hope it helps parents and young people to make more informed choices, both in treatment and in how to live with vitiligo. An informed parent can also help change a child’s future.Sincerely, Taking Action for Vitiligo! Andrew Waters, a dad in the British Virgin Islands whose 10 year old daughter had recently been diagnosed with vitiligo, decided he wanted to make a difference, not only in his daughter's future, but in the future of vitiligo. Andrew told VSI: “When my daughter’s diagnosis was confirmed, I asked myself what I could do to help. I am a keen sailor and so I came up with the idea to sail around the entire British Virgin Islands to raise money for the cause." First Ever Sail-a-thon In what is believed to be the first recorded attempt of its kind, on May 19, 2013, Andrew set sail on a solo-circumnavigation of the 200+ miles around the entire British Virgin Islands. On an IC-24 ‘open cockpit’ keelboat, exposed to the elements for the duration of the non-stop passage, and without any comforts such as a bed, bathroom, or cooking facilities, he completed the journey in just over 24 hours. Andrew's heroic efforts resulted in a donation to VSI in the amount of $5000!
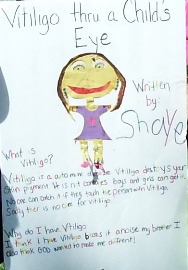
First Vitiligo Walk-a-thon for VSI Many of you have probably noticed the announcements from time to time about the "Dallas/Fort Worth Support Group" meetings. This support group was started a few years ago by two young ladies in middle school, and supported by Dr. Amit Pandya, a dermatologist well known in the vitiligo community. As they have worked at becoming more organized, Sharif Currimbhoy, a clinical research fellow working with Dr. Pandya, contacted VSI seeking ideas for fundraisers that the Dallas support group might do to support VSI. After some discussion, it was decided that they would conduct a "Vitiligo Walk-a-thon!" The walk, held on June 22, 2013, was a great success with more than 70 participants and volunteers in attendance. The total amount raised from business sponsors and individual walkers was nearly $4,300. The walker who raised the most was Shaye East, who had a total of $350.00 in sponsorships! Shaye created a beautiful poster for the Walk-a-thon!
Shaye's words were so special that we wanted to share them with you.
These four issues are responsible in large part for the "access to treatment and care" problems that patients with skin diseases like vitiligo face every day. If you live in the United States and would like to join VSI's "Advocacy Team" to receive advance notice when there is pending legislation that could affect you as a vitiligo patient, click here.
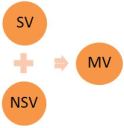
Childhood Vitiligo: Childhood vitiligo is its own unique form of vitiligo with characteristics that set it apart from adult vitiligo. It presents issues that affect treatment selection, coping strategies, and the need for ongoing skin and health monitoring. As a parent, appreciation of these special issues can help your child get the most effective treatment and psychological support. In this article we look at childhood vitiligo, its unique characteristics and treatments, and need for ongoing monitoring. Vitiligo Basics Vitiligo is a chronic disease in which melanocytes (cells that make pigment) in the skin are destroyed, causing the skin to be depigmented. It occurs in adults and children, all races, and both sexes. Its abrupt onset can be at any age. For 50% of people with vitiligo, depigmentation starts before the age of 20; for 25%, under the age of 10. Vitiligo usually depigments only the skin, but it can appear anywhere we have pigment cells, such as the hair (scalp, eyebrows, eyelashes), inside the mouth, retina, ear, and genitals. Though many have no other symptoms, research has shown that at least 20% of those with nonsegmental vitiligo (NSV) experience itching at onset and location of depigmentation. We’ve also recently learned that some with vitiligo develop a mild hearing loss. Vitiligo is a complex syndrome involving multi-causative factors, some of them working in concert. How and why the melanocytes disappear, we do not fully understand. But we do know there is an autoimmune component, as well as genetic and biological factors not yet understood. This autoimmune component plays a central role in the most common form of vitiligo, NSV. This autoimmune link appears to be less a factor in the other two types of vitiligo, segmental (SV) and mixed (MV). Knowing which type of vitiligo a child has is important, as each differs in (1) how it progresses, (2) its response to treatment, and (3) its risk for other autoimmune disease. Nonsegmental Vitiligo (NSV) NSV is considered to be progressive, with cycles of spreading and stability. Though we know there are triggers that can set off the onset or worsening of vitiligo, such as hormonal changes during puberty, skin injury (Koebner phenomenon), emotional stress, and vitamin D insufficiency, we do not yet fully understand the course the disease will take as a child moves into adulthood. As NSV shares common genetic links with other autoimmune disorders, children with NSV have been found to be at risk for other autoimmune diseases, especially autoimmune thyroiditis (AIT). This risk is highest for children who have both a longer history of vitiligo, and a positive family history of thyroid disease. In AIT, the body’s own antibodies target thyroid function, leading to Hashimoto’s thyroiditis (hypothyroidism, or deficient activity) or Graves’ disease (hyperthyroidism, or excessive activity). Other autoimmune disorders reportedly found in children with vitiligo include allergies (most commonly manifested as allergic rhinitis (hay fever), but also as bronchial asthma, atopic dermatitis, or food allergy), alopecia areata, psoriasis, celiac disease, diabetes, and Addison’s disease. Experts universally recommend an annual screening of thyroid function including a complete thyroid panel with the following tests: thyroid stimulating hormone (TSH), Free T3, Free T4, and thyroid peroxidase (TPO). The importance of this screening is underscored by the fact that the risk of thyroid disease, especially for females, increases with age. In addition, some experts recommend diagnostic tests for vitamin D; antinuclear antibody (ANA), which can detect antinuclear antibodies associated with other autoimmune diseases; diabetes; Addison’s disease; and complete blood counts (CBC), which can detect other disorders. Homocysteine levels are also recommended to be evaluated in patients who are on restricted diets, especially vegetarian. Optional tests for folic acid, insulin/glucose, vitamin B6, and vitamin B12 may also be done in selected cases. You can find more detailed information on thyroid disease and vitiligo in VSI's Spring 2010 newsletter. Detailed information about these thyroid and autoimmune tests can be found in the Summer 2011 newsletter. Past newsletters are archived on VSI's Community page. Segmental Vitiligo (SV) SV does not have the strong autoimmune association of NSV. Those with SV have less family history of autoimmune disease, including thyroid disease and vitiligo. However, recent research suggests that in some cases there may be an immune-activated overlap between SV and NSV. This is evidenced by the fact that some SV cases later develop NSV. This combination is then classified as mixed vitiligo (MV), as discussed below.
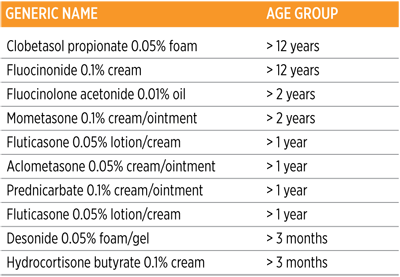
Mixed Vitiligo (MV) In the uncommon cases when SV patients later also develop NSV, it is called mixed vitiligo. Preliminary research indicates that signs of inflammation or autoimmunity such as itching, halo nevi (moles surrounded by a white ring or “halo”), and antithyroid antibodies (such as TPO antibodies) might signal the onset of this type. The risk is greater if the initial segmental vitiligo is on the trunk. How is Vitiligo Diagnosed? Vitiligo is diagnosed by direct observation of the skin, usually by a dermatologist. In those cases where the diagnosis is difficult, a skin biopsy may be taken. In instances where the skin is light and it is difficult to distinguish the lesion from the surrounding skin, a Wood’s lamp (an ultraviolet light used to detect depigmentation) may be used. Testing is also recommended for the presence of autoimmune and thyroid abnormalities and disorders linked to vitiligo. The previously mentioned tests are aimed at identifying antibodies and other markers that are symptomatic of autoimmune disease. Information on having a successful meeting with the physician can be found in VSI's Summer 2010 newsletter. Treatments and Repigmentation The vitiligo treatments used in adults are also used in children, though in some instances in lower dosages to avoid certain side effects in children. However, the treatment goal is the same: to stop the progression of the disease, and then to repigment the skin. Most children with vitiligo have the potential of achieving at least moderate repigmentation with treatment, especially if the disease is treated early after onset. Once complete repigmentation is achieved, treatment can be stopped and resumed if the vitiligo returns. The limited data available makes it difficult to predict how long repigmentation will last. However, we do know that the more stable the vitiligo, and the more complete the repigmentation at the end of treatment, the less chance of relapse in that area. Complete repigmentation is defined as the skin of the repigmented area matching the color of the surrounding skin, with no white remaining at all. Some doctors recommend continuing to treat an area that appears repigmented for an extra month or two to be sure that no depigmentation remains. There is a growing consensus among doctors that early treatment of vitiligo is important not only to ensure the best chance for repigmentation, but also to avoid the permanent depletion of melanocytes in the depigmented area. The longer you wait before treating, the greater the risk of depleting the melanocyte reservoir, which is believed to be the reason why people with long-term vitiligo often have a more difficult time repigmenting. If white hairs are present in the vitiligo lesion, the melanocyte reservoir may be permanently depleted, making repigmentation more difficult. If there are hairs that still have their natural color within the vitiligo lesion, this is generally a good sign that there are remaining melanocytes in the reservoir to support repigmentation. In areas where there are few to no hair follicles, vitiligo can be harder to treat and may require a combination of therapies for enhanced efficacy. For example, vitiligo on the palms, soles, fingertips, toes, lips, mucosal areas, nipples, around the eyes, and anal area may take more time to repigment. Vitiligo lesions on bony prominences like elbows, knees and ankles can be more challenging to treat as well. Treatments Used for NSV Affecting less than 20% of the Body Topical Steroids Topical therapy is the first choice in treating localized or more limited vitiligo. Moderate-high-strength topical steroids are the most popular because they are an established, relatively inexpensive, prescription anti-inflammatory treatment that is easy and convenient to use. Topical steroids are moderately effective in repigmenting the skin, especially on the face, neck and genital areas. Most vitiligo experts will “cycle” between topical steroids and the topical immunomodulators (discussed further on) until maximum repigmentation is achieved in order to minimize side effects and ensure the skin continues to respond to therapy. Thinning of the skin (skin atrophy) is a well-known side effect that can result from application of a high-strength steroid for a prolonged time without a break. Long-term use can also cause permanent stretch marks. All of these risks can be more of a concern when facial or thin-skinned areas are being treated or large areas of skin are treated for long periods of time. If used on large areas of the skin for prolonged periods of time, the potent steroids can be absorbed into the bloodstream causing systemic side effects in other areas of the body, which is why most doctors prescribe intermittent use. Topical steroids have also been used in combination with topical calcipotriene (a vitamin D3 analogue also sold as Dovonex cream) to enhance the efficacy of calcipotriene and reduce the risk of steroid side effects. This combination has been reported to be effective in improving repigmentation results, including in those who had previously failed with topical steroids alone. Oral steroids are rarely used, except as a short course to halt the spread of vitiligo in those older children and adolescents with rapidly-progressing, generalized disease. The chart below shows the more commonly used topical steroids, noting the ages they are typically prescribed for.
Topical Immunomodulators Topical immunomodulators - tacrolimus (sold as Protopic) and pimecrolimus (sold as Elidel) - also known as topical calcineurin inhibitors (TCIs), are often used as alternatives to topical steroids, especially in treating vitiligo on the face, head and neck. TCIs have fewer short-term side effects than topical steroids, though their long-term effects are unknown. Protopic is slightly more effective than Elidel, but both are commonly used. Protopic’s base is like a petroleum jelly ointment, while Elidel’s base is a cream. Research has shown that medication delivered in an ointment base is always more potent than the same medication in a cream base, as an ointment base promotes greater penetration of the medicine into the skin than a cream. However, a cream is best in treating sensitive skin areas such as those involved in the folds of the skin. Elidel has been reported to be beneficial when treating the genitals and the area around the eyes. Some prefer Elidel on the face, as the cream base is less likely to cause acne breakouts than the ointment base of Protopic. Both TCIs have been reported to be helpful in treating those who have failed previous therapies and in treating long-term vitiligo (i.e., those with vitiligo more than five years). Excimer Laser Therapy Targeted light therapy using the 308-nm laser is an effective therapy reserved to repigment limited sites of stable vitiligo as well as for treatment-resistant vitiligo. The therapy offers the advantage of focusing the light at the site of the lesion with minimal side effects and sparing the surrounding skin from light exposure. Published medical tests of this therapy have reported good results for the majority of children, especially on the face, neck and trunk, with repigmentation rates ranging from 50% - 75%. One study with 49 Chinese children also reported that this therapy, used in combination with topical pimecrolimus, produced superior results to the laser light alone, especially on the face. Treatments Used for NSV Affecting Greater than 20% of the Body Narrowband UVB (NB-UVB) Narrowband UVB is the first choice of treatment for widespread NSV childhood vitiligo. It represents a significant advance in treating childhood vitiligo. When delivered to the entire body, it can stabilize and at least moderately repigment the skin in the majority of the children treated. NB-UVB can also be used in combination with topical treatments, including steroids, calcipotriene, and TCIs to enhance efficacy of treatment. Psoralen plus UVA light (PUVA) PUVA was once the gold standard of vitiligo treatment, but is now used less often since the emergence of NV-UVB, due to its side effects. Oral PUVA involves the combination of light and an oral psoralen. It is not used in children under the age of 12 because of its risk of burning, nausea, and cataracts, and only for widespread disease in children 12 and over. Topical PUVA can be used safely to treat localized vitiligo in children at least two years old. Depigmentation Therapy For those who have at least 50% pigment loss, or where the pigment loss is extensive in the more visible areas of the body, and repigmentation therapies have not worked, depigmentation is an option. Depigmentation therapy is used to remove the remaining pigment in the skin to match the areas that are already depigmented. The prescription used to depigment is the topical application of monobenzyl ether of hydroquinone (MBEH) also commonly referred to as monobenzone. This is the only drug approved by the FDA for depigmentation therapy of advanced vitiligo. Typically, a cream with a 20% concentration of MBEH is applied twice a day to limited areas where pigment remains (such as arms, legs, or chest) for 12-18 months. It is important to understand that since this is a systemic treatment, meaning that regardless of where the cream is applied, it will affect the entire body, and areas away from the treated area will still lighten. This is not a treatment used to selectively lighten or depigment a specific or confined area. Treatment will generally begin with a concentration of 20% MBEH, but may be increased to higher strengths later if needed. MBEH is now only available as a compounded product (monobenzone powder added to a base cream) made by specialized pharmacies. While there are periodic shortages of the monobenzone powder, VSI maintains a list of pharmacies where the compounded cream is generally available. While depigmentation is used less often in children, for those with extensive vitiligo who are old enough to be counseled and understand the permanence of the decision, there are doctors who will work with families that make this decision. Segmental Vitiligo Treatments In the past, mainstream therapies were not thought to work well, so surgical therapies such as mini-grafting were considered the most effective therapy. However, as discussed below, recent research is showing quite the opposite, that the more mainstream therapies do work well when used early after onset of SV. Surgical Treatments Blister grafts have been shown to be significantly better in SV than in the NSV and in individuals less than 20 years of age. The child or adolescent selected for this procedure must be able to tolerate the post-operative immobility that may be required during recovery, depending on the location of the vitiligo. The possible need for immobility during recovery, combined with the fact that vitiligo lesions continue to increase proportionately in size as children grow, makes surgical therapy less viable for very young children. Microdermabrasion, an in-office light cosmetic procedure that gently removes the outer layer of skin, has been used effectively in combination with topical Elidel cream to repigment skin. Used together, they were reported to achieve greater than 50% repigmentation in the majority of lesions after three months. This proved superior to using Elidel alone. Topical Therapy and Phototherapy Several of the traditional treatments used in NSV are now being found to be more effective than previously thought in SV, if they are used early after onset. A recent Korean study, for example, found that the excimer laser was more effective in repigmenting the skin in children and adults with SV when used in early stages of the disease. A second group of Korean researchers also observed that those who had SV for five months or less had the best repigmentation results from phototherapy, achieving more than 50% repigmentation. They also found that SV patients responded well to the traditional vitiligo treatments (oral steroids, TCIs, excimer laser + drug therapy) when treated early. Protopic ointment and Elidel cream have also been reported to be effective in pediatric SV patients. In a 2004 study, researchers at Roosevelt Hospital Center in New York City reported that 18 of 21 children with SV responded to 1% Protopic, especially those with facial involvement. They recommended Protopic as a treatment of choice for children with SV of the head and neck. Mixed Vitiligo Treatment MV is a relatively new classification. As a result, treatment data is limited. However, according to one recent study of a small group of MV patients using NB-UVB, the NSV responded well. Because SV of longer duration is generally either slow or non-responsive to non-surgical therapy, the SV was far less responsive to the NB-UVB. You can find detailed information on each of the vitiligo treatments in VSI's Winter 2010 and Spring 2011 Newsletters. Do Children with Vitiligo Need Special Psychological Support? Many children cope well with vitiligo. However, some are more negatively impacted in terms of their self-esteem and overall emotional health. The unpredictable course of vitiligo, the disruption of racial self-perception, and the cosmetic disfigurement can burden these children with psychological difficulties, even into their adulthood. Their feelings of being stigmatized can lead them to conceal their disease and avoid socializing. In surveys about coping with vitiligo, children have expressed worry about the disease getting worse, anger, embarrassment, depression, and shame. Adolescents can also feel general apprehensiveness about the illness, independent of its severity. At an age where teens acutely feel social pressures regarding appearance, vitiligo can be very difficult to deal with. Since stress can trigger or exacerbate vitiligo, it is important for these teens to get emotional support. Treatment and psychological support by family and friends can help a child with vitiligo cope and maintain a good quality of life. Individual counseling by a professional may also be helpful in certain cases. What do I Need to do Going Forward? Staying informed about vitiligo allows you to work with your physician to determine the most effective path for your child. Encouraging your child to also be educated about vitiligo will help him understand the best way to live with a chronic disease. While many young people achieve significant repigmentation through treatment, it takes time and requires persistence. The most beneficial thing you can do is to find a physician who is knowledgeable about vitiligo, who will answer your questions, and work with you. If you can’t find one in your area, consult VSI’s “Doctor Search,” which can be located under the menu tab labeled “Community” after logging onto your account. If there is not a specialist listed for your area, (you can also use the "Search" function to find mentions of cities near yours to see if one is discussed), look online or call around for a physician who will work with you, perhaps even one willing to consult with a vitiligo specialist elsewhere. Young Children Children will vary in how they respond to vitiligo. Some will handle it very well right from the beginning; others may be uncertain and lose confidence, or self-esteem. Children’s attitudes will frequently mirror their parents’. Children will have a better chance of coping if they get positive and encouraging support. If there is anxiety, be reassuring. The younger the child, the less detailed discussion is needed, but be willing to answer questions and acknowledge their feelings. It can also help to meet with your child’s teacher in preschool and kindergarten to help them understand what vitiligo is. This will help the teacher support your child and help the other children understand. One idea is to suggest to As children get older, they may start to notice that their skin is different. It is important for them to understand that everyone has something unique or different about them. Some people may have light skin, others dark skin. Some are short; others are tall. Being different is not a bad thing. Elementary Children
Brainstorming with your child can help him/her develop options for things to say when others ask questions or make comments. Sometimes, in the stress of the moment, it’s hard to come up with a good response, so talking through possibilities ahead of time can help a child feel more prepared. A smile is always a good way to help others focus on that rather than on vitiligo. It can also be helpful to talk about why some children feel the need to be negative or cruel to others – often this is because the child is dealing with self-esteem issues of his/her own, and for whatever reason, it helps to put others down. Understanding this can help your child know that it is more an issue with the other child’s insecurity than with your child’s skin. Talking through responses can empower your child to deal with these issues positively rather than respond in a negative way that only encourages further bad behavior. Teenagers All teens are self-conscious and want to fit in. Parents need to be understanding, especially when new situations create insecurities. By being supportive and encouraging, your teen has a good chance of accepting his/her skin and feeling comfortable with others. Again, if they encounter negative remarks, help them to understand that this reflects others’ insecurities and to not let those remarks have power over them. Just as with younger children, you might practice with your teen on how to handle various negative remarks they might hear so they can practice their response. Be alert to your child’s feelings about having vitiligo and be prepared to provide additional support during difficult times. Monitoring your child’s skin for changes is important to ensure early treatment of new vitiligo lesions. Last, but not least, know that you and your child are not alone. Patients, physicians, and scientists around the world share your concern about vitiligo and are working together to promote the best vitiligo research and care that will lead to a better future!
Insurance Coverage for Vitiligo Treatments VSI is often asked for help when insurance claims for vitiligo treatment are denied. Insurance companies are required to provide the basis (reason), in writing, for any denials. The information VSI provides is geared towards the reason given. The cause for denial that we hear about most often is "cosmetic." Believe it or not, many doctors routinely obtain insurance coverage for vitiligo treatments, even with Medicare claims. Why do so many other doctors experience problems? The doctors who are more successful in obtaining insurance coverage for vitiligo treatments:
Doctors in smaller (or solo) practices may not have the time and/or resources necessary to battle insurance companies. VSI has been asked to help form a task force to identify the problems and create a template that all doctors can use to eliminate this problem. Some insurance carriers are more difficult to work with than others; a carrier can even have different results depending on the state. We'd like to hear about your insurance experiences regarding vitiligo, good and bad. If you are from the USA, please click below to participate in a brief survey to help VSI establish equal access to treatment for all vitiligo patients!
What's On Your Mind? Q. I am completely depigmented and wondered if my skin can still
Q. I had vitiligo, but now seem to have developed alopecia areata, and am losing the hair on some of my vitiligo patches. Is it common to have both conditions on the same location? Will the hair grow back??
Highlights of recently-published medical Scenesse: Follow-up to first "Phase II" Study Very Promising
According to the company, the 41 patients who completed the combination treatment as part of a 6-month Phase II study had more repigmentation at the end of five months following the end of treatment than the group who had been treated with NB-UVB alone. In addition, the repigmentation in the combination group had remained stable since the start of therapy 11 months earlier (6 months of treatment plus five-month follow up period); pigment stability after treatment is often an issue. No significant adverse effects were reported in the combination group by either patients or physicians. At the follow-up, patients said that the treatment was well-tolerated. The combination therapy group was treated 3 times weekly with NB-UVB for 6 months total; starting in the second month, they received a series of 4 monthly implants containing afamelanotide, followed by a final month of NB-UVB monotherapy. The monotherapy group of patients was treated with NB-UVB alone over the 6-month study period. Repigmentation occurred earlier in those on the combination therapy (median 43 days versus 68 days) and those with the darkest skin complexion achieved a deeper and more complete repigmentation compared to those only being treated with NB-UVB. The combination therapy potentially offers a way to achieve faster and greater repigmentation and one that can be maintained without continuing treatment. NB-UVB is the most effective treatment currently available for widespread vitiligo. Its combined use with afamelanotide could be the first choice in treatment in the future. According to Clinuvel’s acting Chief Scientific Officer, Dr. Dennis Wright, “These results, together with the earlier efficacy analyses, show that Scenesse has the potential to become the main pharmaceutical agent used in the treatment of vitiligo.” Clinuvel has announced that it expects to conduct a Phase IIb study of Scenesse in vitiligo in Europe and Asia before the end of 2013, if approved by regulatory authorities.
Study Reveals that Treatment Outcome is Dependent on
To that end, they contacted 101 of their vitiligo patients who had used NB-UVB or PUVA at their hospital between 2007 and 2010 to ask about their treatment compliance, perception of results, and actual results. They received responses from 79 people, 86% of whom were 50 or under. Their analysis was published in a recent issue of the Indian Journal of Dermatology. Questionnaire findings: Of the 79 responding, only 21 were compliant (continued regular phototherapy treatments), with 18 of them under the age of 25, compared to 14 who were under 25 out of the 58 who were non-compliant (those who treated irregularly or stopped hospital treatment). Eighteen of the 21 compliant patients had four or more lesions, including more on the visible areas of the body. Only 22 of 58 non-compliant patients had four or more lesions; 12 had lesions on visible areas. The primary reason given for stopping phototherapy was side effects (22.8%), with nearly half of these patients dropping out during the first four weeks of treatment. The side effects reported were skin redness, itching, burning sensation, blistering, and increased pigmentation of the normal skin. They also cited factors such as the distance they had to travel at least 2-3 times per week for a prolonged period (14.4%), busy schedules (13.4%), and a variety of other reasons such the lack of positive results, lesion repigmentation, few lesions, home treatment, cost, and transportation. Just 4 patients from the compliant group reported negative side effects, compared to 46 of the 58 in the non-compliant group. Conclusions: Higher numbers of young people and those with more extensive and visible disease, especially on the face, were compliant; the researchers theorized they were more "psychosocially" affected and consequently more determined to obtain the maximum results. Those who were older or had less extensive and/or less visible disease were less likely to treat regularly. Side effects and other barriers need to be better addressed to improve compliance. Perception, expectations and faith in treatment: All patients were asked about their expectations of treatment response. All 21 compliant users had faith that the treatment would work, while of the 58 non-compliant users, 22 believed the phototherapy would help, 9 were uncertain, and 27 did not believe phototherapy would work. Conclusions: Patients who dropped out of treatment early were less informed about expectations. Going forward
Clinical Trial in Canada
Editors Note: UVA1 is a relatively new form of phototherapy that has been found to be effective in treating several skin disorders, including atopic dermatitis, localized scleroderma, systemic sclerosis, cutaneous T-cell lymphoma, lupus erythematosus, and others. Side effects (burning, hyperpigmentation, redness, itch, etc.) appear less frequently compared to conventional phototherapy, and none serious that can be traced directly to UVA1 treatment, though long-term studies are not yet available. Instances of UV-induced burning were actually less than with broadband UVB or PUVA treatments. UVA1 is reported to induce immediate tanning and pigment darkening. Responses from UVA1 treatments continue even months after the treatment is completed therefore generally requiring fewer overall treatments. UVA1 units consist of metal halide lamps equipped with special optical filters, which emit longer, more penetrating wavelengths than the fluorescent UVA tubes used with PUVA. Both smaller units to treat localized areas and larger cabinets to treat the whole body are available. Use of UVA1 light units are limited in the U.S., due most likely to the high cost of the equipment, which can be 2-3 times more expensive than conventional whole-body light units.
Paid Study in Detroit Michigan
Your Opportunity to Move Research Forward!
Patients and Controls Invited to
Earn Funding for VSI 3 Ways When You Shop! Please keep VSI in mind when you do any of your online shopping
|
||||||||||||||||||||||||||||
| Copyright © 2013 Vitiligo Support International Inc. All rights reserved. Reproduction or republication strictly prohibited without prior written permission A Vitiligo Support International, Inc. financial statement is available upon written request from the Virginia Office of Consumer Affairs. Mail requests to: Virginia Department of Agriculture and Consumer Services, Office of Consumer Affairs, P.O. Box 1163, Richmond, Virginia 23218. Click here to unsubscribe |
|||||||||||||||||||||||||||||

 Now Visit VSI
Now Visit VSI 








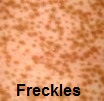 New pigment generally comes from the hair follicle, where the melanocytes reside. It usually begins as a small dot or freckle. It will continue to grow until it eventually fills in the depigmented area. Sometimes the new pigment (freckle) will show up inside a depigmented area, with one or more freckles that grow bigger. Other times, you won’t see any freckles inside the area, but instead the depigmented area gets smaller and smaller because the new pigment is migrating from the outside edges of the depigmented area.
New pigment generally comes from the hair follicle, where the melanocytes reside. It usually begins as a small dot or freckle. It will continue to grow until it eventually fills in the depigmented area. Sometimes the new pigment (freckle) will show up inside a depigmented area, with one or more freckles that grow bigger. Other times, you won’t see any freckles inside the area, but instead the depigmented area gets smaller and smaller because the new pigment is migrating from the outside edges of the depigmented area.